
Dr. Tiffany Cvrkel
As advancements and new technologies are rapidly emerging in health and medicine, there are an increasing number of ethical questions that arise. Dr. Tiffany Cvrkel is a bioethicist, philosopher, and lecturer in UCLA’s Molecular, Cell, & Developmental Biology department. In this week’s interview, she will teach us about the role bioethicists play in doctor and patient lives, and the importance of practicing correct bioethics in all aspects of medicine.
Dr. Cvrkel, how did your interests in philosophy, ethics, and medicine come together?
I have loved science and medicine for a very long time – far longer than I have loved philosophy. Like most American kids, I didn’t even know what philosophy was until I set foot on a college campus. I was utterly seduced by every STEM class I took, and I bounced around from biology to computer science to physics and back to biology. In an alternate universe, I would have probably become a clinician. And then, one day, I found myself in a philosophy class. It was philosophy of medicine, and for the first time, I was pushed to think about medicine in a radically new-to-me way. Philosophy as a field is dedicated to questioning (and on a good day, answering) the foundational assumptions that dwell at the bottom of other inquiries. The field is not unified by subject matter so much as we’re unified by method. Our method is simple and unflinching: one’s claims demand justification.
Our method is simple and unflinching: one’s claims demand justification.
Dr. Tiffany Cvrkel’s Bioethics Tips
nature of health and disease and the purpose of medicine, and I had been taking them all on faith. I wanted to do better. I fell in love with the method, and changed my major to philosophy immediately. In graduate school, I focused on basic questions about praise, blame, and moral responsibility. Like science, ethics is broken down into several subfields. Bioethics is under the umbrella of applied ethics – the solving of particular problems as they exist in the world. My work in grad school was mainly in normative ethics – the theoretical underpinning of ethics. This divide between the applied and the normative is very similar to the divide between applied and basic/pure science. Just like the best applied science researchers have very solid grounding in basic science, I think so too do the best applied ethicists have very solid grounding in normative ethics.

Ethics
Another way to capture this idea is to say that morality is descriptive. It refers to what people actually think or feel or belief. Ethics, on the other hand, typically refers to principles that exist independently (or outside) of what people believe. They are, on this usage, prescriptive – related to how people *should* act or value. I am not sure where these usages originated from, but it was certainly not from those of us who work in this field. Roughly speaking, here’s why. You might believe all kinds of things, for all kinds of reasons. You might believe the world is a week old, or that colds are caused by malicious spirits. And while some fields would be deeply interested in what you believe and how those beliefs developed (maybe psychology and/or anthropology?) your beliefs are not that interesting/helpful to scientists who want to figure out the truth about the age of the world or what causes colds. People in my line of work focus on what is true, not what people believe. We typically use these terms interchangeably to refer to the prescriptive idea, especially since people have been thinking and writing about these notions far longer than the English words have been around. If you read academic ethics, it is best to forget that other disciplines use these words in strange (to people like me!) ways.
Tell us about your current work in bioethics; How different do you think it will be in five years based on trends in science and bioethics?
I joke that my current work is about the very large and the very small. In particular, I am concerned with emerging technologies that allow us to make intentional changes to the germline of an embryo (the genetic information that will be passed on from generation to generation) – that is the very small part – and the developing marriage between medicine, research and Big Data – that is the very large part. These questions are representative of the greatest trend of medicine (and thus bioethics) in our immediate future. For many years, medical technology developed independently of many other forms of technology. We had people solving problems in separate but parallel platforms, and while there have been enormous advances in computing and data processing, those advances haven’t always been directly translated into patient-facing technologies. That is changing. Now, we’ve reached a point where technological advances in RFID might have applications in pacemakers, for instance. It is a very exciting time.
The practice of medicine is about science, yes. But it is also about relationships. We owe it to doctors to teach them these tools, alongside the rest of their training.
How does bioethics directly impact the lives of doctors and patients?
At the most basic level, bioethics helps create the best possible relationship between doctor and patient. Take medical decision making, for example. The patient comes to the doctor because he is in need of help that he is unable to provide for himself. The doctor has years of training and expertise, knowledge that the patient lacks. She knows what interventions statistically bring the best outcomes, at the general population level, but she is not an expert on the patient’s decision-making process. How risk-adverse is he? How might different complications affect him in particular? How is the patient supposed to know enough to ask about what he doesn’t know? We’ve moved past the days when doctors just did whatever they determined was best for a patient without a patient’s consent or input, and rightfully so. But how much information is the doctor supposed to give the patient before she receives genuine informed consent? What if the patient has an irrational fear of needles and refuses to get an infusion that might save his life? What should the doctor do? Bioethics can answer these questions. This field helps both doctors and patients navigate these interactions in respectful, productive, and ethical ways. The practice of medicine is about science, yes. But it is also about relationships. We owe it to doctors to teach them these tools, alongside the rest of their training.
What is an example of an important success story that bioethicists have had in medicine and healthcare in the past decade?
Here are a lot of bioethicists doing good work, but the first person who comes to mind with this question is the work that Margaret O. Little is doing at Georgetown. Little is a philosopher/bioethicist, and her recent work has focused on one of the most difficult and controversial bioethical areas: pregnancy, fetuses, and abortion. A great bioethicist looks at controversies that appear to be at stalemate and identifies how to resolve them. Typically, controversies like stem cell research are at stalemate because both sides are arguing with unfounded assumptions and unsupported rhetoric. They’re talking past each other. Breakthroughs happen when people identify the essential distinctions that have otherwise been missed. Little has so much good work – go read her whole body of writing if you have time! – but one of my favorite pieces of hers is her recent defense of a gradualist view of the moral status of embryos. Many of us have an intuition that an 8-cell pre-implantation embryo is importantly morally different than a 39 week old fetus. But not many of us can argue *why* this might be true. That is what Little does, and she does it beautifully.
are arguing with unfounded assumptions and unsupported rhetoric. They’re talking past each other. Breakthroughs happen when people identify the essential distinctions that have otherwise been missed. Little has so much good work – go read her whole body of writing if you have time! – but one of my favorite pieces of hers is her recent defense of a gradualist view of the moral status of embryos. Many of us have an intuition that an 8-cell pre-implantation embryo is importantly morally different than a 39 week old fetus. But not many of us can argue *why* this might be true. That is what Little does, and she does it beautifully.
Stem Cell
that might allow genomic engineering. Just a few short months ago, the first papers were published about this technology, and there has been a loud call for a standard of ethical conduct for its use. My full view is too long for this space, but the short of it is this: I do not believe that there are ethical reasons to completely prohibit the use of this technology for genomic engineering. Many people have offered arguments that there is something inherently morally problematic with germline engineering, and I argue that those views are not sound. But I do believe that there are particular classes of cases where the application of this technology will be morally problematic, and thus should be restricted. The danger of having ethicists (or lawyers or politicians) who are not trained in the relevant technology making policy on their own is that there is a temptation to play fast and loose with the particulars. The science informs the actual risks, and if you don’t deeply understand the science, you don’t understand the stakes. My job is to work with scientists and researchers to *combine* my expertise with theirs, and this work cannot be done well without the collaboration.
The danger of having ethicists (or lawyers or politicians) who are not trained in the relevant technology making policy on their own is that there is a temptation to play fast and loose with the particulars. The science informs the actual risks, and if you don’t deeply understand the science, you don’t understand the stakes
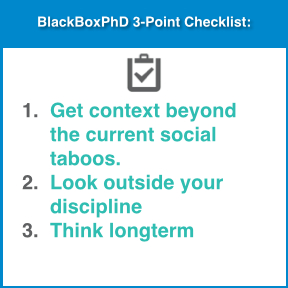
What 3 pieces of advice would you give to someone who is forging new ground by creating a controversial new health technology (for example related to stem cells) and wants to ensure that the technology keeps best ethical practices?
- Don’t start from what’s currently socially accepted (or taboo). Public opinion is fickle and dangerous – many morally horrible things have been publicly embraced over the years (and morally permissible things rejected). Start by identifying the genuine moral concerns in your area, and only then can you start to find solutions to them. None of the people who committed bioethical horrors set out to do evil work. Most stayed within the conventions of their time, but they still did monstrous things. We can (and must) do better.
- Include thinkers outside your discipline. I am a philosopher who works in a hard science department, and my work is so much better for it. It is inevitable that people trained in the same discipline will have the same tendency towards blind spots. It is amazing how much light an outside perspective can bring. This is especially true with including perspectives of people who will be doing most of the patient interfacing, such as nurses. The people who do care delivery at the bedside know things about risks and patient care that very few of us ever learn. This is also where I highly suggest talking to your friendly neighborhood philosopher. We are very good at this work, and generally happy to help.
- Think beyond the short term. Emerging technologies often have uses and implications beyond their immediate goals, and as the developers, you are in a unique position to see into that future. Don’t be surprised by the direction that others might want to take your work. Think about problems that are not yet on the horizon, but might one day come. Ethics is far more pleasant in advance than in retrospect.

Pingback: Oakley Sunglasses Cheap
Pingback: URL
Pingback: waterproofing
Pingback: Dungeon
Pingback: binaural
Pingback: DMPK Services
Pingback: Corporate Event Managers in Hyderabad
Pingback: domino online
Pingback: scr888 download
Pingback: make money with a iphone
Pingback: iraqi coehuman
Pingback: best wedding planners
Pingback: diyala engineer
Pingback: UK Chat
Pingback: 먹튀검증
Pingback: freemoviesz
Pingback: forex signals
Pingback: Christian Louboutin Outlet
Pingback: sport injury clinic
Pingback: smerter
Pingback: forex signals
Pingback: كلية العلوم جامعة ديالى
Pingback: Ambika Ahuja Jaipur Escorts
Pingback: NEHA TYAGI MODEL JAIPUR ESCORTS
Pingback: JAIPUR ESCORTS ALIYA SINHA
Pingback: BANGALORE COMPANION ESCORTS
Pingback: Dhruvi Jaipur Escorts
Pingback: JAIPUR ESCORTS MODEL DRISHYA
Pingback: Heena Khan Bangalore Escorts
Pingback: Jiya Malik High Profile Jaipur Escorts Model
Pingback: FUN WITH JAIPUR ESCORTS PUJA KAUR
Pingback: XXX BANGALORE ESCORTS Rozlyn Model
Pingback: SAPNA CHAUDHARY Escorts in Bangalore
Pingback: Selly Arora Independent Bangalore Escorts
Pingback: Enjoy With Jaipur Escorts Tanisha Walia
Pingback: RUBEENA RUSSIAN BANGALORE ESCORTS
Pingback: Bristy Roy Independent Bangalore Escorts
Pingback: SRUTHI PATHAK MODEL Escorts in Bangalore
Pingback: Bangalore Escorts Sneha Despandey
Pingback: Radhika Apte Model Bangalore Escorts
Pingback: Eva J Law Goa Escorts
Pingback: Fiza Khan Kolkata Escorts Services
Pingback: sbobet game
Pingback: gypsies
Pingback: Ruby Sen Kolkata Independent Escorts
Pingback: Diana Diaz Goa Independent Escorts Services
Pingback: Diksha Arya Independent Escorts Services in Kolkata
Pingback: Devika Kakkar Goa Escorts Services
Pingback: Rebecca Desuza Goa Independent Escorts Services
Pingback: Yamini Mittal Independent Escorts Services in Goa
Pingback: Simmi Mittal Kolkata Escorts Services
Pingback: Kolkata Escorts Services Ragini Mehta
Pingback: Navya Sharma Independent Kolkata Escorts Services
Pingback: browse around here
Pingback: Elisha Roy Goa Independent Escorts Services
Pingback: Alisha Oberoi Independent Escorts in Kolkata
Pingback: Divya Arora Goa Independent Escorts Services
Pingback: Simran Batra Independent Escorts in Kolkata
Pingback: Ashna Ahuja Escorts Services in Kolkata
Pingback: Sofia Desai Escorts Services in Goa
Pingback: Goa Escorts Services Drishti Goyal
Pingback: Mayra Khan Escorts Services in Kolkata
Pingback: Sruthi Pathak Escorts in Bangalore
Pingback: Ambika Ahuja Jaipur Escorts Services
Pingback: Sruthi Pathak Bangalore Female Escorts
Pingback: Sruthi Pathak Bangalore Escorts Services
Pingback: Trully Independent Bangalore Escorts Services
Pingback: Fiza Khan Kolkata Independent Call Girls Services
Pingback: Ruchika Roy Kolkata Escorts Call Girls Services
Pingback: Fiza Khan Kolkata Independent Escorts Call Girls Services
Pingback: Fiza Khan Kolkata Call Girls Escorts Services
Pingback: Diksha Arya Kolkata Escorts Call Girls Services
Pingback: Diksha Arya Kolkata Independent Escorts Call Girls Services
Pingback: klocki lego latarnia morska
Pingback: Cheap
Pingback: Nidika Offer Call Girls in Bangalore
Pingback: Hyderabad Escorts Call Girls Services
Pingback: Pune Escorts Services Call Girls
Pingback: Bangalore Cheap Escorts Sevices
Pingback: Goa Escorts Call Girls